INTRODUCTION
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) was first reported in Wuhan, China in December 2019 and represented the pathogen agent that induced COVID-19. The onset and evolution of COVID -19 is severe when is associated with another comorbidities. Patients with acute leukemia present high risk for severe form of COVID-19
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) was first reported in Wuhan, China in December 2019 and represented the pathogen agent that induced COVID-19. The onset and evolution of COVID -19 is severe when is associated with another comorbidities. Patients with acute leukemia present high risk for severe form of COVID-19
OBJECTIVES
The main objective was to evaluate the particularities of COVID-19 in patients with acute leukemia.
The main objective was to evaluate the particularities of COVID-19 in patients with acute leukemia.
METHOD
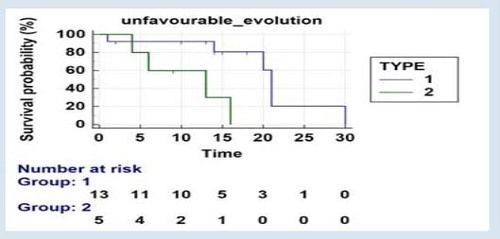
Our study was retrospective and included 49 patients with acute leukemia ( 27 male median age 64 and 22 female median age 54,5) who also were SARS CoV2 positive between April 2020- February 2021 admitted in Hematology and Intensive Care Unit Departments of Colentina Clinical Hospital Bucharest. The diagnosis was established using molecular test for SARS-Cov2. Severe forms of COVID-19 or the presence of newly diagnosed acute leukaemia were predictive factors for adverse outcomes (hospitalization in ICU 12.03, p = 0.0005 Exp (b) = 20.95 95% CI of Exp (b) = 3.75-116.9, acute onset leukaemia Wald 8.24, p = 0.004, Exp (b) = 49.5, 95% CI of Exp (b) = 3.45-709.77). Patients with ALL had a shorter survival curve compared to patients with AML, Chi-squared = 7.37, p=0.007 Fig.3.
Our study was retrospective and included 49 patients with acute leukemia ( 27 male median age 64 and 22 female median age 54,5) who also were SARS CoV2 positive between April 2020- February 2021 admitted in Hematology and Intensive Care Unit Departments of Colentina Clinical Hospital Bucharest. The diagnosis was established using molecular test for SARS-Cov2. Severe forms of COVID-19 or the presence of newly diagnosed acute leukaemia were predictive factors for adverse outcomes (hospitalization in ICU 12.03, p = 0.0005 Exp (b) = 20.95 95% CI of Exp (b) = 3.75-116.9, acute onset leukaemia Wald 8.24, p = 0.004, Exp (b) = 49.5, 95% CI of Exp (b) = 3.45-709.77). Patients with ALL had a shorter survival curve compared to patients with AML, Chi-squared = 7.37, p=0.007 Fig.3.
RESULT
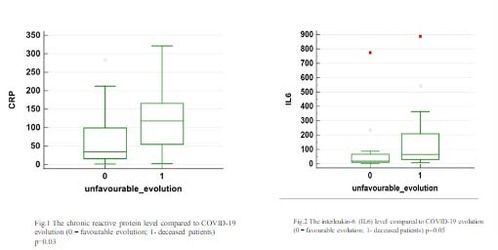
In the group was included 32 patients diagnosed with acute myeloid leukemia (AML), 9 patients with acute lymphoid leukemia (ALL), 6 patients with acut promyelocytic leukemia and 2 patients with acute bifenotypic leukemia. Severe form of COVID-19 with ICU addmission was diagnosed in 16 patients (32,17%), almost all of them (15 patients) had unfavourable evolution compared with non-ICU patients group with only 1 deceased patient, p<0.0001. The recent chemotherapy followed by severe aplasia was the main negative factor that impacted patient evolution (rho=0.508, p=0.0002), 13 patients admitted in ICU Department and 12 patients in non-ICU. Severe pneumonia (more than 30% lung field) was diagnosed in 17 patients with recent chemotherapy and 4 untreated patients. The type of leukemia or refractory status have not any impact of patient evolution. Antiviral therapy – Remdesivir rapidly introduced in patient’s therapy was followed by favourable evolution. Patients with unfavourable outcomes had significantly increased median values of C-reactive protein, procalcitonin and interleukin 6: CRP 117.98 mg / dl (min 2.22, max 321.32) vs 34.45 mg / dl (min 1.55, max 284.18) p0.03 Fig.1; procalcitonin 0.29 mg / dl (min 0.07, max 12.6) vs 0.04 mg / dl (min 1.55, max 8.23) p0.01; IL6 65.27 pg / ml (min 8, max 887.9) vs 18.46 mg / dl (min 1.5, max 774.2) p0.05 Fig.2 The remaining haematological, biochemical and coagulation parameters are not significantly different between groups identified by the type of evolution of COVID-19 (favourable/unfavourable).
In the group was included 32 patients diagnosed with acute myeloid leukemia (AML), 9 patients with acute lymphoid leukemia (ALL), 6 patients with acut promyelocytic leukemia and 2 patients with acute bifenotypic leukemia. Severe form of COVID-19 with ICU addmission was diagnosed in 16 patients (32,17%), almost all of them (15 patients) had unfavourable evolution compared with non-ICU patients group with only 1 deceased patient, p<0.0001. The recent chemotherapy followed by severe aplasia was the main negative factor that impacted patient evolution (rho=0.508, p=0.0002), 13 patients admitted in ICU Department and 12 patients in non-ICU. Severe pneumonia (more than 30% lung field) was diagnosed in 17 patients with recent chemotherapy and 4 untreated patients. The type of leukemia or refractory status have not any impact of patient evolution. Antiviral therapy – Remdesivir rapidly introduced in patient’s therapy was followed by favourable evolution. Patients with unfavourable outcomes had significantly increased median values of C-reactive protein, procalcitonin and interleukin 6: CRP 117.98 mg / dl (min 2.22, max 321.32) vs 34.45 mg / dl (min 1.55, max 284.18) p0.03 Fig.1; procalcitonin 0.29 mg / dl (min 0.07, max 12.6) vs 0.04 mg / dl (min 1.55, max 8.23) p0.01; IL6 65.27 pg / ml (min 8, max 887.9) vs 18.46 mg / dl (min 1.5, max 774.2) p0.05 Fig.2 The remaining haematological, biochemical and coagulation parameters are not significantly different between groups identified by the type of evolution of COVID-19 (favourable/unfavourable).
CONCLUSION
Patients with acute leukemia are negatively impacted by intensive chemotherapy during COVID-19 evolution. The key for good prognosis of these patients during COVID-19 are rapid diagnosis and antiviral therapy at the onset of the disease.
Patients with acute leukemia are negatively impacted by intensive chemotherapy during COVID-19 evolution. The key for good prognosis of these patients during COVID-19 are rapid diagnosis and antiviral therapy at the onset of the disease.
REFERENCES
Paul S, Rausch C, R, Jain N, Kadia T, Ravandi F, DiNardo C, D, Welch M, A, Dabaja B, S, Daver N, Garcia-Manero G, Wierda W, Pemmaraju N, Montalban Bravo G, Thompson P, Verstovsek S, Konopleva M, Kantarjian H, Jabbour E: Treating Leukemia in the Time of COVID-19. Acta Haematol 2021;144:132-145. doi: 10.1159/000508199
.Vikas Mehta, Sanjay Goel, Rafi Kabarriti, Daniel Cole, Mendel Goldfinger, Ana Acuna-Villaorduna, Kith Pradhan, Raja Thota, Stan Reissman, Joseph A. Sparano, Benjamin A. Gartrell, Richard V. Smith, Nitin Ohri, Madhur Garg, Andrew D. Racine, Shalom Kalnicki, Roman Perez-Soler, Balazs Halmos and Amit Verma, Case Fatality Rate of Cancer Patients with COVID-19 in a New York Hospital System, Cancer Discov July 1 2020 (10) (7) 935-941; DOI: 10.1158/2159-8290.
Liu J, Li S, Liu J, Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS- CoV-2 infected patients. EBioMedicine. 2020 May; 55: 102763, Published online 2020 Apr 18. doi: 10.1016/j.ebiom.2020.102763
Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 Apr 6;46(5):846–848, doi: 10.1007/s00134-020-05991-x
5. Robert G Uzzo, Alexander Kutikov, Daniel M Geynisman, et al COVID-19: Risks for infection, clinical presentation, testing, and approach to infected patients with cancer, ed. UpToDate. Waltham, MA: UpToDate Inc. https://www.uptodate.com (Accessed on 02 Apr, 2021.)
Paul S, Rausch C, R, Jain N, Kadia T, Ravandi F, DiNardo C, D, Welch M, A, Dabaja B, S, Daver N, Garcia-Manero G, Wierda W, Pemmaraju N, Montalban Bravo G, Thompson P, Verstovsek S, Konopleva M, Kantarjian H, Jabbour E: Treating Leukemia in the Time of COVID-19. Acta Haematol 2021;144:132-145. doi: 10.1159/000508199
.Vikas Mehta, Sanjay Goel, Rafi Kabarriti, Daniel Cole, Mendel Goldfinger, Ana Acuna-Villaorduna, Kith Pradhan, Raja Thota, Stan Reissman, Joseph A. Sparano, Benjamin A. Gartrell, Richard V. Smith, Nitin Ohri, Madhur Garg, Andrew D. Racine, Shalom Kalnicki, Roman Perez-Soler, Balazs Halmos and Amit Verma, Case Fatality Rate of Cancer Patients with COVID-19 in a New York Hospital System, Cancer Discov July 1 2020 (10) (7) 935-941; DOI: 10.1158/2159-8290.
Liu J, Li S, Liu J, Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS- CoV-2 infected patients. EBioMedicine. 2020 May; 55: 102763, Published online 2020 Apr 18. doi: 10.1016/j.ebiom.2020.102763
Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 Apr 6;46(5):846–848, doi: 10.1007/s00134-020-05991-x
5. Robert G Uzzo, Alexander Kutikov, Daniel M Geynisman, et al COVID-19: Risks for infection, clinical presentation, testing, and approach to infected patients with cancer, ed. UpToDate. Waltham, MA: UpToDate Inc. https://www.uptodate.com (Accessed on 02 Apr, 2021.)
The data in this poster was presented at EHA 2021. Published with permission from the Copyright owner.
